Advances in medicine and healthcare, even in the last 50 years, are far too numerous to name. People live longer, healthier lives than at any time in modern history. Treatment for mental health disorders, as well as substance abuse and addiction, has also benefitted from these advances.
Cognitive Behavioral Therapy and Dialectical Behavior Therapy are evidence-based approaches for treating addiction and mental health issues, such as anxiety, depression, or borderline personality disorder.
The National Alliance on Mental Illness estimates 37 percent of people battling alcoholism and 53 percent of individuals coping with drug addiction suffer from at least one serious mental illness.
CBT and DBT have been shown to be effective in the treatment of both addiction and mental health issues. So, what’s the difference and how do they work?
Cognitive Behavioral Therapy
Cognitive Behavioral Therapy is among the most widely practiced types of therapy used by psychologists and psychiatrists. Patients that undergo this therapy learn the relationship between their thoughts, feelings and behaviors and how each component influences the other.
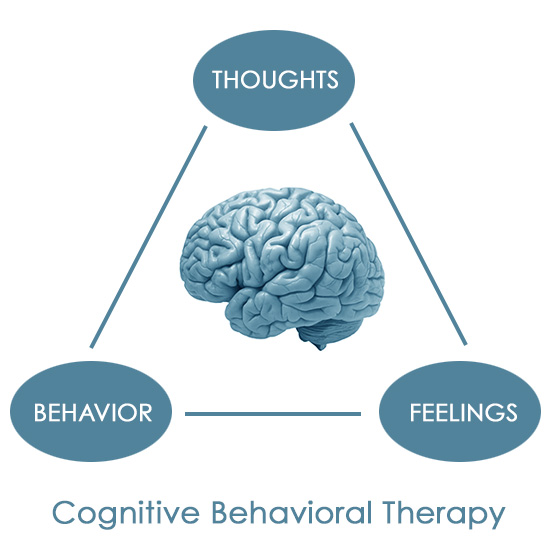
- If a person believes that no one loves them (thoughts), it can lead to depression and loneliness (feelings), which might cause them to avoid interaction with others or refuse to develop deep relationships (behavior).
Over time and in a limited number of one-on-one sessions, CBT allows individuals to recognize, manage, and adjust thoughts that lead to painful or destructive outcomes. Learning to live and think in completely new ways is empowering and effective.
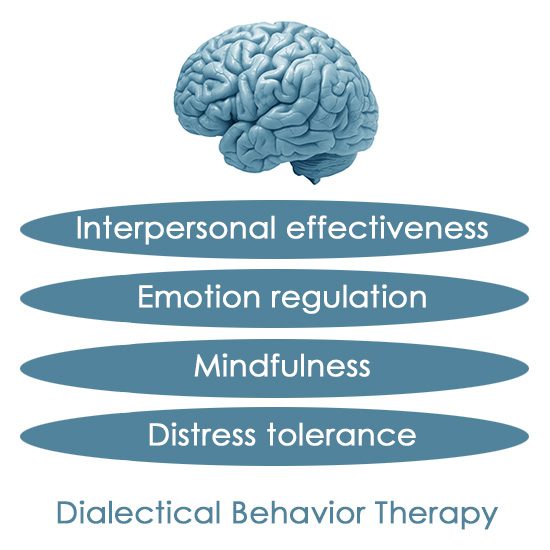
Dialectical Behavior Therapy
Dialectical Behavior Therapy is a branch of CBT. In fact, the creator of cognitive behavioral therapy originally developed DBT to augment its effectiveness with borderline personality disorder—patterns of thoughts and feelings that drastically affect a person’s ability to function in everyday life. Today, it’s used to treat a broader spectrum of mental health issues.
With DBT, the emphasis is on the social and emotional aspects of day-to-day living. In addition to one-on-one counseling, there’s generally a group therapy session held on a weekly basis. Group sessions are especially important because they’re a guided, safe environment for individuals to develop skills in these four areas:
- Interpersonal effectiveness
- Emotion regulation
- Mindfulness
- Distress tolerance and reality acceptance skills
Not everyone experiences emotions in the same way. For some people, emotions escalate faster than what might seem normal to others. It’s not difficult to imagine how painful and difficult it is for a person to experience such intense feelings constantly.
DBT provides a skill set for patients to accept who they are, manage their emotions, and be aware of their behavior and adjust it when appropriate.
Mental Health and Addiction can be Intertwined.
Mental health, substance abuse, and addiction very often go hand in hand. A longtime battle with addiction changes a person’s brain chemistry and can lead to depression and anxiety.
On the flip side, the painful symptoms of a psychiatric disorder can cause a person to self-medicate in an effort to regulate or escape their emotions.
It’s not always clear which came first for a person, but addressing both issues in treatment is vital for a successful recovery. Since no two people are alike, CBT and DBT are adjusted to meet each patient’s individual needs.
Deciding which is most effective is determined through discussions with a therapist.
It’s important to remember that addiction and mental health issues are treatable and manageable. While there’s often shame attached to these conditions, society is coming to understand that any related stigma is misplaced.
CBT and DBT are advancing in treatment and are powerful tools to jumpstart the healing process.
Related:
What are 5 Strategies of Motivational Enhancement Therapy?
The Benefits of Journaling and Writing Therapy
10 Must-Read Books About Mental Health